Choosing the right respiratory device
+

When it comes to selecting the right respiratory protection there are some important factors to consider: Knowledge of the existing contaminants, application requirements, respirator limitations and the protection levels each offers. Sound complicated? You are not alone, Dräger has the right tools to support you and will help you every step of the way.
Lets look at the approvals of the systems mentioned above:
Daily use
All over the world, many different standards and approvals
Our experts take these regulations into account during the whole lifecycle.
Each filter is CE-certified in accordance with the valid version of EN 14387, EN 143:2000 or the DIN 58620 for CO filters.
Further local approvals are available for some of our X-plore filters, e.g. EAC (Russia), LA (China), NBR (Brazil), SANS (South Africa)
EN 14387. Standard for gas and combination filters
EN 143. Standard for particle filters
DIN 58620. Standard for CO filters
AS/NZS 1716. Australian standard
Filtered escape devices
Two main standards are applicable for the PARAT escape hood series:
DIN 58647-7 for filtering escape devices and EN 403:2004 for fire escape hoods.
In addition, the filters of the PARAT 4700 and 7500 are tested in accordance with EN 14387:2004.
The filter of the PARAT 5500 fire escape hood is additionally tested for the use against H2S (at 2,500 ppm) in accordance with DIN 58647-7.
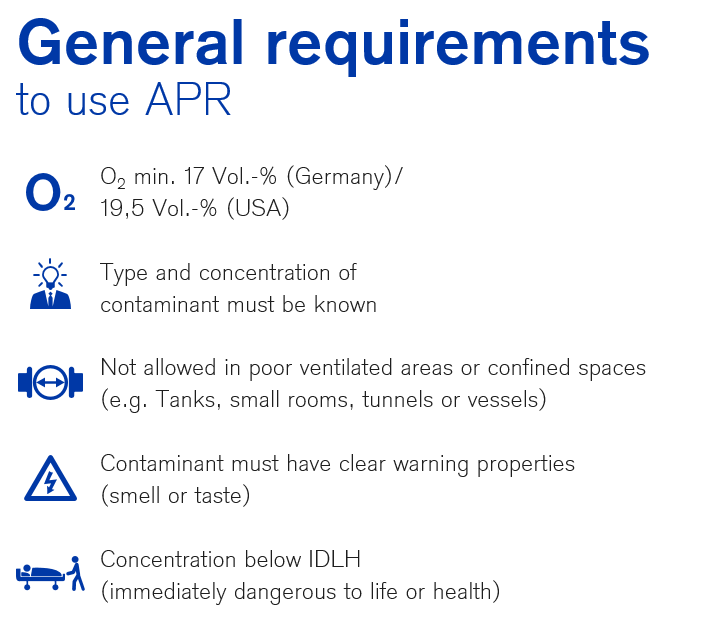
Air purifying respiratory protection
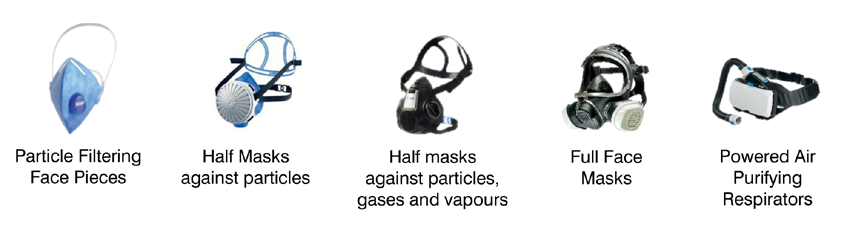
X-plore filters can be used with half masks X-plore 3000 or with full-face masks X-plore 5500 and X-plore 6000.
In addition, Rd40 filters can be used with any half and full-face mask with a standard filter connection. Dräger also offers disposable particle filtering face pieces and even powered air purifying respirators.
Applications for the X-plore Filters

Equipment for fast and safe escape
Emergencies need an expert:
Unplanned situations with hazardous substances can occur within seconds. No escape scenario is the same.
Individual situations need individual escape concepts fitting to your company’s environment.

Applications for the Parat filtered escape devices

Day to day use
The broad portfolio of X-plore filters offers high protection against almost every hazardous substance, including CO* and radioactive methyl iodide*. In total more than 70 different filters are available.
Effective protection against hazardous substances when working with wood, Laboratory work, Painting and Welding as examples. You have to protect your respiratory organs against a diverse range of gases.
*Only Rd40 filter series
Filtered Escape devices
When every second counts, ready for escape in only 3 steps. This saves valuable seconds in emergencies; during maintenance operations, for fire fighters in case of fire to rescue people from the affected area, protection against carbon monoxide during operational use and when fire related and industrial gases might be present at the same time.
Follow the links below for more information on our X-Plore filers and our Parat escape devices;

Day to day Use: https://www.draeger.com/en_za/Safety/Respiratory-Protective-Equipment
Escape and rescue: https://www.draeger.com/en_za/Productselector/Rescue-and-Escape?page=1&i=safety
- Published in Uncategorized
Burnt alive!
Why are workers still being killed in factory fires in Bangladesh?

It is hard to believe that employers and factory owners in Bangladesh still lock fire doors and prevent workers from escaping in the event of a fire.
Eight years ago in 2013, I wrote a damming article about the criminal activities of Bangladesh employers, and the government.
Why is it that eight years later I am asking “How long will it be until factories in Bangladesh manufacturing goods for Canada, the U.S. and European-headquartered companies are safe for workers? Why am I writing about another 52 workers who died in another factory fire in Bangladesh on July 8th, 2021? How can it be in this day and age factory owners are still locking doors preventing workers from escaping fire?
At the Hashem Food and Beverage factory in Rupganj, an industrial town 15 miles east of Dhaka, 52 workers, including children as young as 11, died in a massive fire that began on July 8 and raged on for more than a day, according to a report from Al Jazeera.
The news outlet reported that Jayedul Alam, police chief for Narayanganj district where the factory is located, said the entrance had been padlocked at the time of the blaze and the factory breached multiple fire and safety regulations. A fire services spokesman also said the exit door to the main staircase had been padlocked. Highly flammable chemicals and plastics had also been stored in the building.
If this sounds all too familiar, Bangladesh, which employs tens of thousands of low-paid workers making garments for large international companies has a long and tragic history of industrial disasters.
Continuing corruption and a lack of enforcement have resulted in hundreds of deaths over the years. It is widely believed that the only way to prevent these criminal acts is to boycott clothing produced in Bangladesh.
After the horrific collapse of the Rana Plaza garment factory during 2013 that killed more than 1,100 people, the country imposed tougher safety rules. An agreement between Bangladeshi unions and international brands was signed – The Accord on Fire and Building Safety in Bangladesh. It was a five-year agreement signed in May 2013 and extended until 2018. The next expiry date is August 31, 2021.
According to Remake, the initial inspection of Bangladesh’s factories in 2013 found “more than 87,000 safety issues, including more than 50 factories that were at immediate risk of collapsing”. Since then, as a result of 38,000 initial and follow-up inspections, more than 90% of the original hazards which were identified have been eliminated.
While this is an important step, there are still issues. If there weren’t issues, we wouldn’t see headlines like these with regularity “the country’s garment industry has since become largely compliant under domestic and global watchdogs. But many other local industries fail to maintain safety compliance and the disasters have continued”.
In 2019, 67 people were killed when a complex housing warehouses, shops and apartments caught fire.
Responding to this latest tragedy the International Labor Association gave this statement:
“This incident illustrates the urgent need in Bangladesh for authorities and building owners to ensure that buildings in which thousands of workers spend the better part of their day are built and operated in compliance with national code requirements. If the fire safety measures required by the regulations were properly implemented, it would provide for the safe evacuation of occupants in this type of emergency”.
This cannot and should not ever happen again. Tighter regulations must ensure worker’s safety and we should never have to write another story like this.
When the people take back the power and hold public officials accountable, then and only then, will conditions change. In 1991, after the Imperial Chicken processing plant caught fire in Hamlet, North Carolina in which 25 people were killed, the owner did just under 4 years in prison because he had ordered the doors padlocked from the outside. It was not nearly enough, but it was the first time in North Carolina that someone did real prison time for safety violations.
This was a time of reckoning for NCs safety programmes. Laws were passed, people were held accountable. The feds threatened to take over North Carolina Labor unless certain minimum standards were implemented and John C. Brooks, Labor Commissioner at the time, lost the next election. Since 2004, North Carolina has been ranked in the top 5 safest states to work.
- Published in Uncategorized
Burnt Alive
Why are workers still being killed in factory fires in Bangladesh?

It is hard to believe that employers and factory owners in Bangladesh still lock fire doors and prevent workers from escaping in the event of a fire.
Eight years ago in 2013, I wrote a damming article about the criminal activities of Bangladesh employers, and the government.
Why is it that eight years later I am asking “How long will it be until factories in Bangladesh manufacturing goods for Canada, the U.S. and European-headquartered companies are safe for workers? Why am I writing about another 52 workers who died in another factory fire in Bangladesh on July 8th, 2021? How can it be in this day and age factory owners are still locking doors preventing workers from escaping fire?
At the Hashem Food and Beverage factory in Rupganj, an industrial town 15 miles east of Dhaka, 52 workers, including children as young as 11, died in a massive fire that began on July 8 and raged on for more than a day, according to a report from Al Jazeera.
The news outlet reported that Jayedul Alam, police chief for Narayanganj district where the factory is located, said the entrance had been padlocked at the time of the blaze and the factory breached multiple fire and safety regulations. A fire services spokesman also said the exit door to the main staircase had been padlocked. Highly flammable chemicals and plastics had also been stored in the building.
If this sounds all too familiar, Bangladesh, which employs tens of thousands of low-paid workers making garments for large international companies has a long and tragic history of industrial disasters.
Continuing corruption and a lack of enforcement have resulted in hundreds of deaths over the years. It is widely believed that the only way to prevent these criminal acts is to boycott clothing produced in Bangladesh.
After the horrific collapse of the Rana Plaza garment factory during 2013 that killed more than 1,100 people, the country imposed tougher safety rules. An agreement between Bangladeshi unions and international brands was signed – The Accord on Fire and Building Safety in Bangladesh. It was a five-year agreement signed in May 2013 and extended until 2018. The next expiry date is August 31, 2021.
According to Remake, the initial inspection of Bangladesh’s factories in 2013 found “more than 87,000 safety issues, including more than 50 factories that were at immediate risk of collapsing”. Since then, as a result of 38,000 initial and follow-up inspections, more than 90% of the original hazards which were identified have been eliminated.
While this is an important step, there are still issues. If there weren’t issues, we wouldn’t see headlines like these with regularity “the country’s garment industry has since become largely compliant under domestic and global watchdogs. But many other local industries fail to maintain safety compliance and the disasters have continued”.
In 2019, 67 people were killed when a complex housing warehouses, shops and apartments caught fire.
Responding to this latest tragedy the International Labor Association gave this statement:
“This incident illustrates the urgent need in Bangladesh for authorities and building owners to ensure that buildings in which thousands of workers spend the better part of their day are built and operated in compliance with national code requirements. If the fire safety measures required by the regulations were properly implemented, it would provide for the safe evacuation of occupants in this type of emergency”.
This cannot and should not ever happen again. Tighter regulations must ensure worker’s safety and we should never have to write another story like this.
When the people take back the power and hold public officials accountable, then and only then, will conditions change. In 1991, after the Imperial Chicken processing plant caught fire in Hamlet, North Carolina in which 25 people were killed, the owner did just under 4 years in prison because he had ordered the doors padlocked from the outside. It was not nearly enough, but it was the first time in North Carolina that someone did real prison time for safety violations.
This was a time of reckoning for NCs safety programmes. Laws were passed, people were held accountable. The feds threatened to take over North Carolina Labor unless certain minimum standards were implemented and John C. Brooks, Labor Commissioner at the time, lost the next election. Since 2004, North Carolina has been ranked in the top 5 safest states to work.

By Dr Bill Pomfret
- Published in Uncategorized
Now from Marcé – 4×4 CAFS Pumper
Engine: 326HP/240Kw EURO3 – 1250Nm Transmission: ZF 9S-1310
Marcé body cab with integrated crew cab and equipment lockers. The spacious crew cab provides seating for four crew members including gear and each seating position is equipped with a (BA) Breathing Apparatus seat allowing quick access and fitment of BAs.

The Unique design of the Marcé body or superstructure allows for six spacious lockers that can be easily reached by means of a drop-down step allowing the fire fighter to reach the required equipment. The equipment is safely stored inside the compartments by means of durable aluminium roller shutter doors each fitted with central locking controlled from within the vehicle cab.
The water and foam carrying capacity is 3000L and 300L.
The compact PTO driven multi pressure rear mounted fire pump has a maximum low pressure flow of 6000 litres per minute and maximum high pressure flow of 770 litres per minute. The maximum low pressure is 17 bar and maximum high pressure is 54.5 bar.
The pump is also fitted with two very unique foam systems namely a (CAFS) Compressed Air Foam system and electronic (ATP) Around The Pump foam system.

A Compressed Air Foam System simultaneously attacks all sides of the fire triangle.
• Penetrates and soaks the fuel
• Decreases the fuel’s exposure to oxygen
• Adheres to surfaces to reduce heat
Attacking a fire using CAFS reduces the amount of time to knockdown a fire by as much as 5 times over plain water. This equates to less fire fighter exposure, less water usage, less harmful runoff, and less required overhaul. There are multiple advantages for the front line fire fighter. CAFS helps keep them safer in the hostile environment of a fire scene and reduces attack times, reduces flashover, reduces hose line weight, and reduces exposure and fatigue.

The CAFS system ..balancing the water pump, foam system, and air system so they work effectively together. The CAFS procedure is simplified by fully programmable presets allowing the fire fighters to set CAFS configurations for numerous fire scenarios repeatedly with a single touch. The simplified operation allows changes to the CAFS consistency that is available at the push of a button. A twin-screw rotary air compressor delivers air flow volume of 200 SCFM (in metric terms – 5760 l/min) to match the pump.
The Smart ATP foam system is an intelligent, automated around-the-pump foam system that delivers high-volume, precise foam for every fire situation therefore eliminating the problems with traditional manual systems. The Smart ATP automatically regulates the foam ratio control valve, reducing the opportunity for operator error and wasted foam. Foam ratio percentage can be adjusted from 0.1% to 10% suitable for ARFF, Industrial, structural and Wildland Forestry fire fighting applications.
The vehicle is also equipped with an extremely durable deck monitor (water cannon) that is both wired and wireless providing improved performance and operator control. The maximum flow rate is 5000LPM. The monitor is programmable for STOW, DEPLOY and OSCILLATION, programmable travel limits and keep out zones as well as travel speeds. The monitor is mounted on a electrical actuated extender designed to provide better clearance for the monitor which allows for a wider coverage range and addresses firefighter safety concerns. The Extender deploys in 10 seconds and extends a full 457mm.
In addition to the two CAFS outlets, two water outlets and monitor outlet there is also two electric rewind hose reels capable of reaching pressures in excess of 45bar. Each hose reel is fitted with 45m long high pressure hose and an adjustable pistol grip firefighting nozzle.
- Published in Uncategorized
POPIA Compliance – EMS Buyer’s Guide
The Emergency Services Yearbook & Buyer’s Guide would love to continue sharing our news with you, however, we value your privacy and are committed to following the regulations and requirements of POPIA. If you would rather not receive news or further correspondence from us anymore, please click the unsubscribe at the bottom of this email.
Your consent, and data security and privacy are of upmost important to us. We are fully POPIA compliant and follow all the stipulated regulations to ensure data confidentiality. We will never share your any of your information or details with any third parties.
If you would like to remain on our mailing list no action is required.
Please note that you can opt out at any time by unsubscribing.
- Published in Uncategorized
Emergence of Delta variant substantially increases risk of COVID-19 transmission
Dr Richard Friedland, chief executive officer of Netcare, recently confirmed that the surge in COVID-19 cases and high admissions to hospitals in Gauteng are directly linked to the emergence of the Delta variant in South Africa.

“Initial modelling suggested that Gauteng would experience a third wave, which would be lower than the second wave but may last longer, in other words, the so-called ‘lower for longer scenario’. This appeared to be the case until the first week of June 2021, when the daily number of positive cases started to break the trend, rising exponentially on 15 June. Since then, it has been increasing rapidly – far exceeding the peak of both the first and second waves in Gauteng. Data released on Tuesday, 29 June 2021, confirms that the Delta variant was responsible for 53% of cases sampled in early June and 75% towards the end of June,” notes Dr Friedland.
“The Delta variant is approximately 50-60% more transmissible than the Beta variant, which was responsible for the second wave in South Africa. This explains the mounting surge in cases and admissions to hospitals. Netcare is currently caring for over 2 600 COVID-19 patients across its hospitals in Gauteng. This is 45% higher than the 1 792 patients we had at the peak of the second wave, and almost 100% higher than the 1 377 patients admitted during the peak of the first wave in Gauteng.
“It also explains why we have seen whole families, school-going children, and younger people testing positive and why we have now seen the admission of patients in their in their twenties and thirties affected by the virus,” he added.
“The new COVID-19 Delta variant has been detected in at least five provinces and is now the dominant strain in South Africa. Netcare therefore welcomes the adjusted level 4 measures announced by President Cyril Ramaphosa, as this should have a material impact in helping to curtail the further spread of COVID-19 in the coastal regions, while aiding in flattening the curve.
“We however remain extremely concerned about the current situation in densely-populated Gauteng, and while these restrictions may have come too late to flatten the curve in the province, it will certainly lessen the number of infections and admissions to hospitals,” explained Dr Friedland.
Given the Delta variant’s increased transmissibility, it is now more important than ever to practise safe social distancing, fastidious attention to the wearing of masks, regular washing of hands, the use of sanitiser and avoiding social gatherings. In the absence of a completed vaccine rollout we must rely on the strictest possible non-pharmaceutical preventive measures.
“Vaccination remains a vitally important step in the fight against COVID-19, and it is crucial that individuals are registered and vaccinated as soon as they become eligible. Now, more than ever before, given the emergence of the highly contagious Delta variant, it is critical that everyone takes COVID-19 extremely seriously,” urged Dr Friedland.
Vaccination has thus far proved to be extremely effective in protecting our frontline workers. Of over 33 000 Netcare frontline workers vaccinated only 206 or 0.6% have experienced a breakthrough infection and of them, only seven required hospitalisation.
Extensive, additional preparations are ongoing at Netcare
As a result of the prevalence of the highly transmissible Delta variant, we have further strengthened and adapted our approach to ensure that we are ready, ahead of a potential surge in other provinces, to deal with the new risks in the most effective and efficient way,” he added.
Dr Friedland says Netcare’s preparations for the expected surge, especially in coastal areas, are focused on several key aspects, including additional measures to help safeguard its healthcare workers, optimising capacity to meet the demand for hospital care for COVID-19 patients, procuring additional life-saving equipment, and ensuring sufficient consumables including pharmaceutical stock.
Optimising capacity to prepare for a surge in COVID-19 patients
“We have already started scaling down on non-urgent surgery and medical admissions in our coastal hospitals, and some have suspended such surgery to rapidly create capacity for the expected increased COVID-19 patient numbers. To free up beds for COVID-19 patients, only medically necessary, time sensitive surgeries (MeNTS) will continue, based on the MeNTS scoring system, as well as emergency admission of non-COVID-19 patients,” explains Dr Friedland.
To create further capacity, plans are also in place to convert certain Medicross day theatres and other facilities to accommodate COVID-19 patients, if needed.
“Our clinical resources are being further strengthened by recruiting additional resident medical officers and clinical associates to provide continuous cover in COVID-19 zones. Several specialists have also responded to our call to join the COVID-19 teams in providing care to patients, as locally determined by hospital management and the COVID-19 clinical teams.
“To alleviate the expected pressure on our emergency departments [EDs] and to start treatment of patients as soon as possible, we will be establishing clinical decision units [CDUs] at our coastal region hospitals as a matter of urgency, in addition to those we have implemented in Gauteng. The CDUs are run and managed by the ED doctors and staffed separately from the hospitals and each consists of a number of beds, its own ablution facilities, PPE donning and doffing area and independent oxygen supply for each bed,” he adds.
Procuring additional life-saving equipment and consumables
“In addition to our already high number of ventilators and high flow nasal equipment, Netcare has procured further equipment in preparation to provide the appropriate level of care to COVID-19 patients.
“We have secured over 1 000 more mobile oxygen concentrators to bolster our fleet of 1 400 oxygen concentrators. These machines filter surrounding air, compressing it to the required density to deliver a continuous stream of purified medical grade oxygen to the patient. Importantly, this oxygen is produced without having to rely on the piped oxygen at our hospitals, thus not denuding existing oxygen capacity at the hospitals.
“In addition, we have procured another 100 ventilators, including 40 transport ventilators, which can also be used by emergency medical services personnel when transporting patients in need of oxygen. We continue to boost our extensive oxygen supply with additional bulk tanks.
Safeguarding our frontline heroes
“It is, as always, crucial to safeguard all persons working in our hospitals to the best of our ability. To reduce the footfall in our hospitals and the exposure risk this poses to healthcare workers, we have suspended visitation of patients in our Gauteng hospitals, as well as in a few of our other hospitals, unless for compassionate reasons or in exceptional circumstances.
Keeping lines of communication open
“We have employed more social workers within our facilities to counsel patients and their next-of-kin and loved ones. Next-of-kin of patients to our hospitals are encouraged to call the Netcare Family Connect Line on 0800 111 266, and one of our trained call centre professionals will facilitate a dedicated hospital representative to provide them with personal feedback daily on how their loved one in hospital is doing.
“We are glad to note that many family members are now making use of this special service to maintain contact with their loved ones. This past week alone we have connected more than 1 000 individuals with their loved ones, and we strongly encourage members of the public to avail themselves of this service.
“We wish to assure the public that we will continue to do the very best we can for all patients seeking care at any of our healthcare facilities, while ensuring their safety and that of our frontline heroes,” says Dr Friedland.
Help us to help you
“Despite the pressures placed on us, providing care is our calling, it is our driving purpose, and we are privileged to be serving our country and its people at this challenging time. In doing so, we respectfully appeal to our fellow South Africans to help us in providing them with the best possible care if they need it.
“Test for COVID-19 if you are concerned that you may have contracted the virus and seek care from your general practitioner early if you feel unwell. Many persons unfortunately still wait until their condition becomes a life-threatening emergency, which does not only endanger them but places further pressure on emergency medical services, emergency departments and hospitals,” concludes Dr Friedland.
- Published in Uncategorized
COJ – Your local fire station
Join us on a voyage down memory lane.
In our first post, we will take you to the Brixton Fire Station.
Pictures supplied by Howard Leadbeater






- Published in Uncategorized
Our personal experiences with COVID
By Leighton Bennett, Chairman of the Safety First Association
Both my wife and I have been hospitalised due to Covid and this first-hand experience has prompted me to write about the experience, as there is a general perception that this Covid virus pandemic is a joke. Let me tell you it is a horrific and tragic survival experience I will never ever forget.
I got home last week after a week in high care and am now slowly recovering and gaining strength.

My wife was discharged and got home two days ago, after spending 29 days in hospital. She will still need several more weeks in recovery before she will be able to work again.
Both of us run businesses, a cat hotel (cattery) and my OHS consulting business. We adopted and followed all the Covid virus management safety protocols and still we don’t know how we got infected.
My wife’s Covid experience
It started with my wife not feeling well on a Friday and she went for a nasal Covid test which recorded Covid Negative, but over the weekend she felt terrible with a dry cough, chest pains and breath shortness. I took her to her doctor on Monday who, based on her symptoms said she has asthma, Covid and an x-ray confirmed pneumonia in the lungs. She was medicated and sent home to recuperate.
By Thursday midday her oxygen in the blood reading was 86% where it should be over 93%. I rushed her to the doctor who ordered an ambulance with oxygen cylinder to transport her directly to one of the northern suburbs hospitals. Some four hours later I phoned the hospital to be told she was not admitted to the cited hospital, neither was she answering her cellphone. Where was she? I was extremely worried. When I had last seen her, she she was in a shocking condition trying to breathe and she was not mentally present. The psychological and emotional stress hit me badly. I immediately thought that she is not in hospital as she has died and is now lying in a mortuary somewhere.
At 19h30 that evening my wife’s friend managed to get hold of her. She was in casualty on oxygen at another northern suburb hospital. Absolute relief after I had suffered hours of mental anguish.
The reality is that the hospital’s don’t have any Covid spare beds so you will be sent anywhere where a bed may be available. When I went into hospital some 10 days later, they were planning to send me to a hospital in Klerksdorp, when a northern suburbs hospital high-care bed became available for me.
Hospitals are currently over-flowing with 3rd wave Covid patients and are now forced to apply survival triage Covid case management. This is where a Covid patient may not be admitted into ICU if his or her chance of survival is limited, whereas others will be if they have a better chance of survival. This is not a story, this is the realty that doctors are forced to make, life and death decisions not daily but hourly, during their long 20 hour day on shift when they see some 120 patients per day.
My wife’s condition went from casualty, to a Covid ward, to high care, to sedation on a ventilator in ICU all in under 24 hours. Her condition got to a stage that she had multiple body function failures, namely asthma, Covid, pneumonia, water accumulation surrounding and interfering with her heart function, a collapsed lung, kidney and liver failure and suddenly elevated blood sugar levels due to the medication clash between the Covid and diabetes control medications. My wife actually died and with adrenalin injected into the heart and heart massage, she became a miracle who managed to survive. She later reported hearing the staff order a body bag for her.

Currently her body is like a laptop that has just being rebooted, where everything has to be re-switched on and re-connected. She had to learn to walk again and was on a high litres/minute oxygen supply to get plus 93% oxygen into her blood stream. She only got home after she could breathe the normal 21% oxygen in the atmospheric air for a day or two, and she was not allowed home until we had an oxygen cylinder supply at home, for emergency purposes. Should a relapse occur, she would not be readmitted to hospital as there are no beds available with the Covid 3rd wave happening now.
My Covid experience
My Covid experience started over the weekend after my wife went into hospital. I felt unwell, had a dry cough and such severe leg and calf cramps that I couldn’t sleep for three nights. I went for a throat Covid test on Sunday which was negative. I went to see my doctor on Monday who, based on my symptoms, said I have a false negative Covid test and prescribed antibiotics, nebulizing, heavy vitamin doses and Ivermectin for a week. As the week ended, I was weak, had lost my appetite and started feeling physically useless.
On Tuesday evening my son took me to hospital where I lay in casualty overnight breathing oxygen. The next morning they started searching for a Covid bed for me. I was lucky to get a bed at a northern suburbs hospital where an x-ray confirmed I had a bacterial lung virus which only tested positive for Covid on the 7th Covid test. I went straight into a Covid ward and was then moved to a medical ward as all my Covid tests were still negative, and then a positive Covid test resulted in my medical ward mate being placed in Covid isolation and me relocated to the Covid high-care/ICU ward. This was an adapted maternity ward that had been converted to a Covid beds ward to provide more beds space.
Mornings and evenings, two bags of meds were delivered for the hospital pharmacy to give me three intravenous high dose steroids and vitamin drips that made my hand tremble like I was having Parkinsons. I was originally on 4l/min oxygen allowing me to get the 93% blood oxygen level required to breath safely. I later went off oxygen altogether when I could breathe atmospheric air for three days before being discharged.
A serious complication is that the Covid medication clashed with my diabetic sugar level control medication such that my sugar levels went up to 28.6 (with a likely diabetic coma at 32).
I am now home but still struggling to re-control my diabetes sugar levels condition with blood sugar testing every 3-4 hours currently. In hospital I was getting diabetic insulation pen in-stomach injections for up to 18 insulation units at least twice per day with on-going regular blood sugar tests.
The Covid ward reality
Over and above our Covid experience one needs to know the life and death drama playing out each day in the Covid wards.
Both northern suburb hospitals that we were admitted to have converted their maternity wards into Covid high-care and ICU wards.

The doctors look like astronauts in filtered air-fed face helmets, while all the medical staff are totally covered in Covid blue clad body PPE, face shields, face masks, gloves (changed per patient), foot sleeves, etc, and all are exhausted from the long hours they are working. The medical staff are a crew of “Blue Angels”. Medical hazard waste boxes are everywhere.
The real struggle is seeing an ICU sister tending to a patient on a ventilator desperately trying to breathe and only able to draw 20 to 30% oxygen into their blood stream, where normal breath requires over 93% oxygen in the blood. Regular dry coughing episodes end in a situation of total fatigue and no energy.
No hospital visits are allowed so you don’t know the condition of your significant other or family member, especially if they are ventilator sedated to stop them pulling out the ventilation piping. To make things worse, there is no cell phone communication. You feel totally cut-off.
This is another psychological and emotional stress as you may not be able to “say good bye” or be able to be with or support them at the crucial moment.
Conclusion
My wife and I know five people who have died from Covid – both cattery clients and friends. Hopefully no more will occur. Both our businesses have been closed for over two months now and will only reopen when we have recovered and regained enough strength to be able to function again.
I decided to share our experiences as too many people have no understanding how horrific the Covid pandemic is.
I hope our experiences have given you a revised view of this virus and the importance to practice safe Covid management techniques and methods.
Please don’t take chances.
- Published in Uncategorized
Testing the functionality and tightness of respiratory protection devices
Dräger Quaestor and Testor test devices are highly efficient test benches that test the integrity and therefore the safety of full-face respirators.
Automatic test programmes reduce the time needed to test each full-face mask and valves, and also diving equipment.
Dräger Testor 2500/3500

Versatile testing options
Both Dräger Testor 2500/3500 models are designed for tests in the low and medium-pressure range. They are especially suitable for testing:
‒ full face masks,
‒ compressed air breathing apparatus,
‒ lung demand valves, and
‒ chemical protection suits. Comfort is a matter of position
Realistic mask testing
The test head of the Testor 2500/3500 has a natural shape. It is securely mounted, and the gel face may be replaced independently by the user as required. The design eliminates the need for any inflation and deflation of the test head.
The new gel face II is more robust due to the optimised material composition. This enables full breathing protection masks to be tested faster and better in less time.

Integration is possible in any workshop
With its compact size and robust design, the Dräger Testor 2500/3500 fits into any workshop. A base plate (optional) also enables the device to snap onto the workbench mounting of the Dräger Quaestor 5000/7000 and the Prestor 5000.
The gel face II is used for all three testing device types. This ensures maximum compatibility and increases the efficiency of your workshop.
Dräger Quaestor 7000
All static and dynamic tests of the Dräger Quaestor 7000 are carried out fully automatically. Controlled by the newly developed software, each test is carried out intuitively. For the user this guarantees high efficiency through comfort and speed.
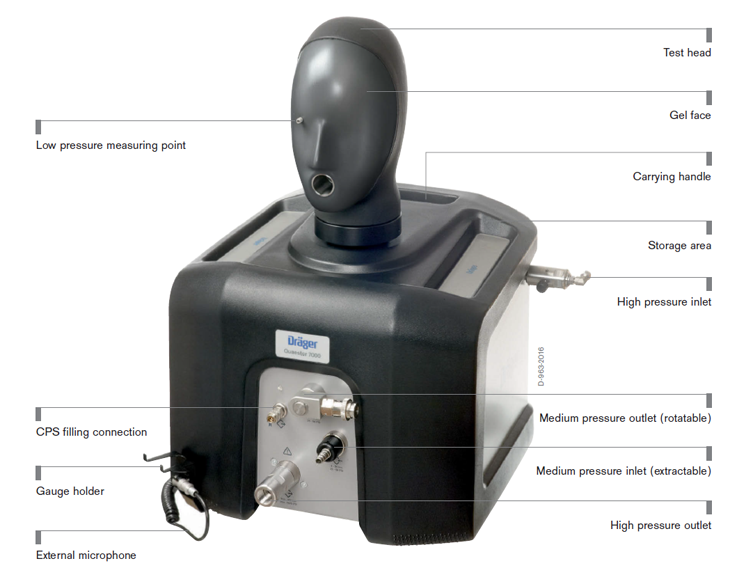
Fully-automatic static and dynamic tests
The test process is fully automated. Automatically opening and closing valves accelerate the process and
manual intervention is no longer required. An external microphone also automatically captures the switchon
point of the low pressure warning. Thus the service technician can use the time during the test for other activities.
Optimum tight fit for all mask sizes
The test head can be turned without restriction and removed as required. This flexibility allows the user to tailor the test design even more individually and comfortably to his requirements. In addition, the gel face of the test head which emulates the elasticity of the human facial skin optimizes the tight fit for all common mask sizes.

Learn more here : https://www.draeger.com/en_za/Productselector/Workshop-Solution-and-Breathing-Gas-Supply/Test-Equipment?page=1&i=safety
Focus product
Dräger Aerotest® 5000
You can use the mobile Dräger Aerotest® 5000 to test the purity of the breathing air in a low pressure system (or in a high pressure system, if you have the right accessories) in accordance with your country’s standards. The automatic system significantly improves ease of use. Menu-guided measuring, data downloads, and printing of test certificates: testing and documentation are easier with the Dräger Aerotest® 5000.
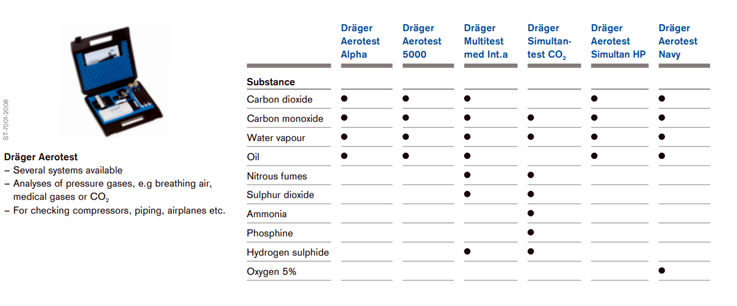
Learn more: https://www.draeger.com/en_za/Products/Aerotest-5000
- Published in Uncategorized


























